When Are Flat Feet a Problem?

Flat feet, or pes planus, is a common condition where the arches of the feet collapse, causing the entire sole to touch the ground. It affects approximately 20 to 30 percent of the population and can occur in both children and adults. Flat feet may develop due to specific factors, including genetics, weak foot muscles, injury, or certain medical conditions. People at higher risk include those with family history, obesity, diabetes, or who stand for long periods of time. There are different types of flat feet. Flexible flat feet are where the arches only flatten when weight is applied. Tight Achilles tendon limits foot movement. Posterior tibial tendon dysfunction is when the tendon supporting the arch becomes weakened. Treatment by a podiatrist aims to relieve painful symptoms and improve foot function. This may involve custom orthotic devices, stretching exercises, supportive footwear, or in severe cases, surgery to reconstruct the arch. If you have problematic flat feet, it is suggested that you schedule an appointment with a podiatrist for proper management and relief.
Flatfoot is a condition many people suffer from. If you have flat feet, contact one of our podiatrists from Ankle & Foot Care Center. Our doctors will treat your foot and ankle needs.
What Are Flat Feet?
Flatfoot is a condition in which the arch of the foot is depressed and the sole of the foot is almost completely in contact with the ground. About 20-30% of the population generally has flat feet because their arches never formed during growth.
Conditions & Problems:
Having flat feet makes it difficult to run or walk because of the stress placed on the ankles.
Alignment – The general alignment of your legs can be disrupted, because the ankles move inward which can cause major discomfort.
Knees – If you have complications with your knees, flat feet can be a contributor to arthritis in that area.
Symptoms
- Pain around the heel or arch area
- Trouble standing on the tip toe
- Swelling around the inside of the ankle
- Flat look to one or both feet
- Having your shoes feel uneven when worn
Treatment
If you are experiencing pain and stress on the foot you may weaken the posterior tibial tendon, which runs around the inside of the ankle.
If you have any questions please feel free to contact our office located in Jupiter, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Flat Feet
Flatfoot is a foot condition in which the arch of the foot has either partially or totally dropped or has never developed. While it is common in babies and small children, it can become a problem for them in adulthood if the arch never forms. For adults, the development of flat feet can be brought upon by injury, as a result of pregnancy due to increased elasticity, or obesity. Those who have health concerns such as rheumatoid arthritis or diabetes may also be at greater risk for developing the condition.
If you suspect that you have flat feet, it is best to consult your podiatrist. Your foot doctor will examine the suspected foot and observe how it looks while you sit and stand. He or she may take an X-ray to determine how serious the condition is. Some common signs of flatfoot include toe drift, in which the toes and front part of the foot point outward, a short Achilles tendon, and a heel that tilts outwardly while the ankle tilts inward.
Once flatfoot has been diagnosed, your podiatrist may suggest one of several treatment options. Flat feet can be rigid, in which the feet appear to have no arch even when the person is not standing; or flexible, in which the person appears to have an arch while not standing, but once standing the arch disappears. Those with flexible flatfoot may be told to reduce any activities that cause pain and to avoid extended periods of walking or standing. Another suggestion may be weight loss, as excessive weight may be placing pressure on the arches
In few cases, if the condition is severe and all other methods have been exhausted surgery may be required. This is normally avoided, however, due to a lengthy recovery time and high cost.
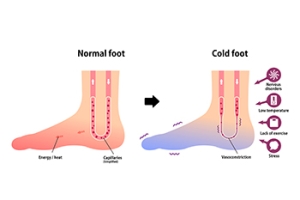
Causes of Chronic Cold Feet
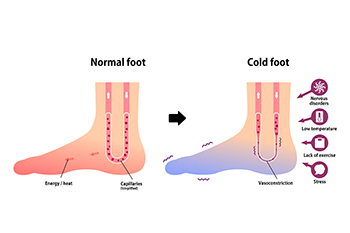
Finding the cause of cold feet is important for both comfort and overall health. While environmental factors may contribute to occasional coldness in the extremities, persistent cold feet could indicate underlying issues. One major issue is poor circulation, often linked to heart conditions, sedentary lifestyles, or smoking. Iron-deficiency anemia is another common cause of cold feet, necessitating dietary changes and supplementation. Diabetes, particularly types 1 and 2, can lead to cold feet from nerve damage, underscoring the importance of blood sugar management. Further, hypothyroidism, peripheral vascular disease, Raynaud’s phenomenon, and arteriosclerosis can all contribute to cold feet. If you are experiencing recurrent cold feet or associated symptoms, like numbness or tingling, it's suggested that you make an appointment with a podiatrist for an evaluation, diagnosis, and treatment options.
While poor circulation itself isn’t a condition; it is a symptom of another underlying health condition you may have. If you have any concerns with poor circulation in your feet contact one of our podiatrists of Ankle & Foot Care Center. Our doctors will treat your foot and ankle needs.
Poor Circulation in the Feet
Peripheral artery disease (PAD) can potentially lead to poor circulation in the lower extremities. PAD is a condition that causes the blood vessels and arteries to narrow. In a linked condition called atherosclerosis, the arteries stiffen up due to a buildup of plaque in the arteries and blood vessels. These two conditions can cause a decrease in the amount of blood that flows to your extremities, therefore resulting in pain.
Symptoms
Some of the most common symptoms of poor circulation are:
- Numbness
- Tingling
- Throbbing or stinging pain in limbs
- Pain
- Muscle Cramps
Treatment for poor circulation often depends on the underlying condition that causes it. Methods for treatment may include insulin for diabetes, special exercise programs, surgery for varicose veins, or compression socks for swollen legs.
As always, see a podiatrist as he or she will assist in finding a regimen that suits you. A podiatrist can also prescribe you any needed medication.
If you have any questions, please feel free to contact our office located in Jupiter, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Causes, Symptoms, and Treatment of Poor Blood Circulation in the Feet
Poor blood circulation in the feet and legs is often caused by peripheral artery disease (PAD), which is usually the result of a buildup of plaque in the arteries. Plaque buildup, or atherosclerosis, can be the result of excess calcium and cholesterol in the bloodstream. This restricts how much blood can flow through arteries. Reduced blood flow to a certain area of the body severely limits the amount of oxygen and nutrients that part of the body receives. This leads to degeneration in the muscles and other tissues. Sometimes, poor blood circulation in the feet and legs can be caused by other conditions, such as the damaging or inflammation of blood vessels, known as vasculitis.
The lack of oxygen and nutrients caused by poor blood circulation can restrict muscle growth and development, as well as cause muscle pain and cramps, weakness, and stiffness. Other common symptoms include numbness in the legs and feet, skin discoloration in the affected limbs, slower nail and hair growth, and erectile dysfunction in men. In more severe cases of PAD, pain can be present even when a person isn't exercising, and may range from mildly uncomfortable to completely debilitating.
Poor blood circulation in the feet and legs is more common in those who are overweight or obese, have diabetes, high blood pressure, high cholesterol, who smoke, or who have a family history of PAD or related conditions such as a heart attack, stroke, etc. Diabetes and smoking place a person at greatest risk for developing poor blood circulation, although advanced age, over 50, can also increase risk.
If you are experiencing poor blood circulation in the feet and legs caused by PAD, it is important to make changes to your lifestyle in order to reduce your risk of experiencing a heart attack or stroke caused by this condition. If you smoke, quit completely. This will increase the amount of oxygen in your bloodstream. Exercising and reducing the saturated fats in your diet. Saturated fats come from fatty meats, fried foods, whole milk, etc., can make a difference in improving blood circulation in feet. It is also important to avoid developing influenza and to carefully control your blood sugar if you have diabetes.
Your doctor may recommend combining lifestyle changes with a prescription medication regimen to improve blood circulation. The most commonly-used medications for PAD are called statins and work by blocking the amount of enzymes in your body that produce cholesterol. They are known by the brand names Zocor, Lipitor, Crestor, and others.
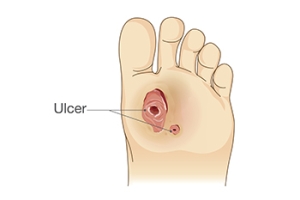
Staying Abreast of Diabetic Foot Ulcer Treatments
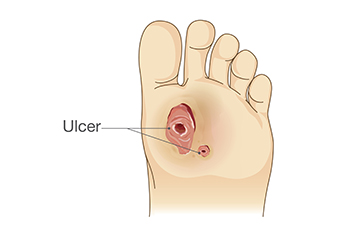
Staying informed about diabetic foot ulcer treatments is necessary for effective patient care. Common interventions include surgical debridement to remove necrotic tissue, antibiotic therapy to combat infection, and vascular assessment to optimize blood flow. Offloading pressure from affected areas is essential for healing. In severe cases, amputation may be necessary to prevent further complications. Additionally, various therapies exist for non-healing wounds, such as advanced dressing. Podiatrists play a vital role in diabetic foot ulcer management, possessing specialized education and skills in this field. By staying abreast of evolving treatments and leveraging multidisciplinary approaches, they can enhance outcomes and improve the quality of life for individuals with diabetic foot ulcers. If you suffer from diabetic foot ulcers, it is strongly suggested that you make routine appointments with a podiatrist for the best care possible.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with one of our podiatrists from Ankle & Foot Care Center. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our office located in Jupiter, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
Dealing With an Ankle Sprain

Ankle sprains occur when the ligaments in your ankle are stretched or torn beyond their intended limits, leading to varying degrees of pain and swelling. Ankle sprains are typically categorized into three grades, ranging from mild stretching to full tearing of ligaments, with Grade III sprains often requiring medical intervention, such as a brace or in some cases, surgery. While certain self-care measures help to ease symptoms, seeking expert care from a podiatrist is essential for a proper diagnosis, treatment, and prevention of chronic ankle sprains. A podiatrist may recommend using splints, casts, or braces, along with rehab exercises to aid in recovery and prevent future sprains. It is especially important to monitor symptoms closely and seek medical attention if pain persists or worsens, or if there are signs of numbness, weakness, or other concerning symptoms. With proper care and guidance from a podiatrist, most ankle sprains can heal effectively. If you have a sprained ankle, it is suggested that you seek immediate attention from a podiatrist who is trained to deal with this injury.
Although ankle sprains are common, they aren’t always minor injuries. If you need your ankle injury looked at, contact one of our podiatrists from Ankle & Foot Care Center. Our doctors can provide the care you need to keep you pain-free and on your feet.
How Does an Ankle Sprain Occur?
Ankle sprains are the result of a tear in the ligaments within the ankle. These injuries may happen when you make a rapid shifting movement while your foot is planted. A less common way to sprain your ankle is when your ankle rolls inward while your foot turns outward.
What Are the Symptoms?
- Pain at the sight of the tear
- Bruising/Swelling
- Ankle area is tender to touch
- In severe cases, may hear/feel something tear
- Skin discoloration
Preventing a Sprain
- Wearing appropriate shoes for the occasion
- Stretching before exercises and sports
- Knowing your limits
Treatment of a Sprain
In many cases, the RICE method (Rest, Ice, Compression, and Elevate) is used to treat ankle sprains. However, you should see a podiatrist to see which treatment option would work best with your injury. In severe cases, surgery may be required.
It is important to ask your doctor about rehab options after you receive treatment for your injury. Stretching, strength training, and balance exercises may help the ankle heal while also preventing further injury.
If you have any questions, please feel free to contact our office located in Jupiter, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Ankle Sprains
Although ankle sprains may not be as serious as a broken ankle, they should be given immediate attention and care. An ankle sprain can lead to a significant amount of pain, as well as limited mobility. They are often characterized by the swelling and discoloration of the skin. This occurs when the ligaments are stretched beyond their limits.
The simple act of walking can sometimes cause a sprain, which makes ankle sprains a very common injury that can happen to anyone. They occur when the ankle twists in an awkward way or rolls over itself, causing a pop or snap in the tendons around the ankle. Some people are more at risk than others. These include athletes who continually push their bodies to the limits and also people who have previously suffered accidents to the feet, ankles, or lower legs.
Most of the time, an ankle sprain is not severe enough for hospital attention. There are many at-home treatment options available, including propping the leg up above your head to reduce blood flow and inflammation, applying ice packs to the affected area as needed, taking over-the-counter pain relievers and anti-inflammatory medication, using an ACE bandage to wrap and support the injured ankle, and most importantly, remaining off your feet until the ankle has fully healed.
Despite this, an ankle sprain can turn into a severe injury that might require hospitalization. If the ankle ligaments or muscles are damaged from a tear or rip, that is one sign that the sprain is severe enough for hospital attention and possibly for surgery. Even after the surgery, the recovery process can be long. You may need to have rehabilitation sessions administered by your podiatrist to get your ankle back to full health.
The severity of your sprain might become apparent if you are unable to stand or walk, consistent pain occurs over a prolonged period of time, swelling is much more severe than initially present, or if you start to experience tingling or numbness. These signs may indicate that your ankle sprain might actually be a broken ankle, an injury that requires immediate medical attention.
Although they are not completely avoidable, ankle sprains can be curbed with some preventative treatment measures. These include wearing appropriate-fitting shoes that not only provide a comfortable fit, but also ankle support. It is also recommended to stretch before doing any kind of physical activity, as this will help lower your body’s chance for an injury.
Heel Pain From Bursitis

Heel pain can be caused by bursitis, which is a painful swelling of the small fluid-filled sacs called bursae. These bursae act as cushions, reducing friction between tissues such as tendons, ligaments, and bones. When they become inflamed, the result is heel pain and limited mobility, particularly in areas like the back or bottom of the heel. Bursitis typically develops due to repetitive movements or prolonged pressure on a joint. Aging also can lead to the breakdown of the bursa over time. Symptoms often include dull pain, tenderness, and stiffness near the affected area. Swelling and redness may also be present, indicating inflammation. Diagnosing bursitis involves a thorough examination by a podiatrist. After a physical examination of the affected area, further tests such as X-rays, MRI scans, or ultrasound may be necessary. If you are experiencing unexplained heel pain, it is suggested that you schedule an appointment with a podiatrist who can determine if you may be suffering from bursitis.
Many people suffer from bouts of heel pain. For more information, contact one of our podiatrists of Ankle & Foot Care Center. Our doctors can provide the care you need to keep you pain-free and on your feet.
Causes of Heel Pain
Heel pain is often associated with plantar fasciitis. The plantar fascia is a band of tissues that extends along the bottom of the foot. A rip or tear in this ligament can cause inflammation of the tissue.
Achilles tendonitis is another cause of heel pain. Inflammation of the Achilles tendon will cause pain from fractures and muscle tearing. Lack of flexibility is also another symptom.
Heel spurs are another cause of pain. When the tissues of the plantar fascia undergo a great deal of stress, it can lead to ligament separation from the heel bone, causing heel spurs.
Why Might Heel Pain Occur?
- Wearing ill-fitting shoes
- Wearing non-supportive shoes
- Weight change
- Excessive running
Treatments
Heel pain should be treated as soon as possible for immediate results. Keeping your feet in a stress-free environment will help. If you suffer from Achilles tendonitis or plantar fasciitis, applying ice will reduce the swelling. Stretching before an exercise like running will help the muscles. Using all these tips will help make heel pain a condition of the past.
If you have any questions please contact our office located in Jupiter, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.